
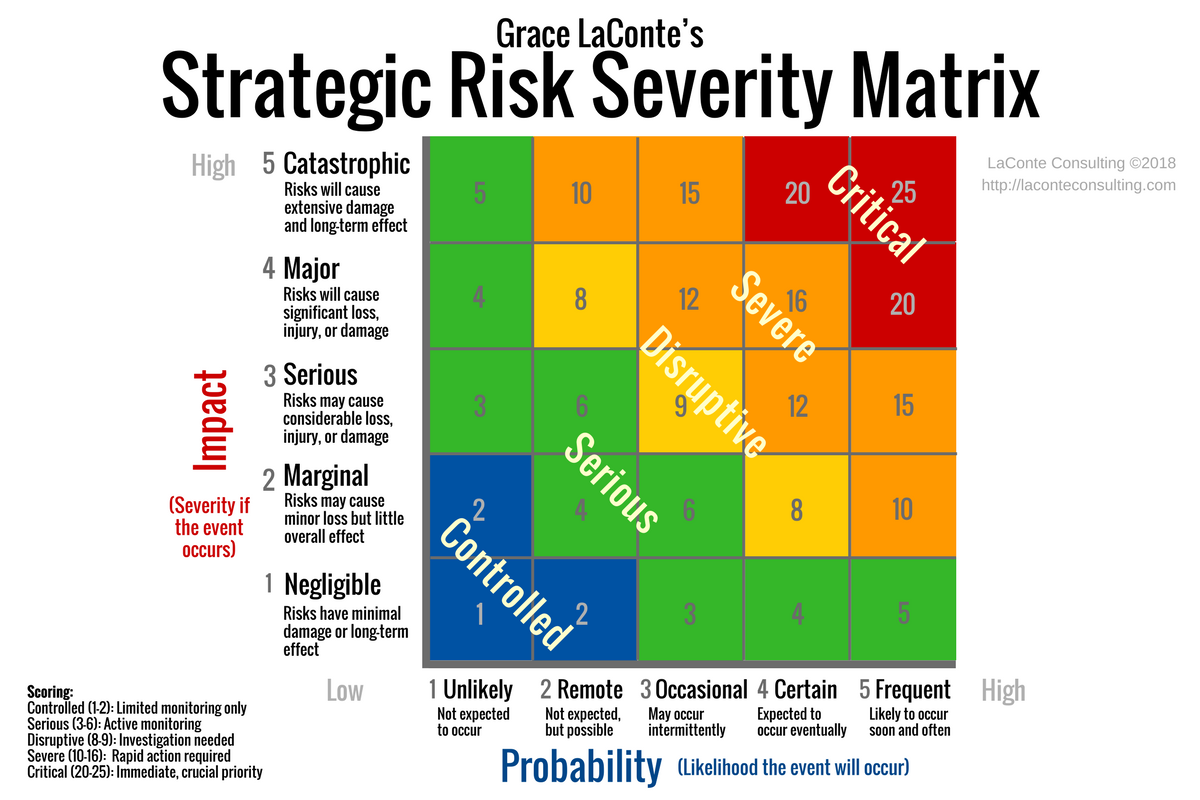
We evaluated the effect of interventions and diagnostic thresholds on risk, using a risk matrix approach (RMA), and factors influencing the decision-making process towards the development of new guidelines and protocols.Ī group of obstetric professionals ( n = 131) participated from 2013 to 2016 in a guideline development project in the catchment area of the tertiary Maastricht University Medical Center, the Netherlands. The aim of any risk evaluation tool is to ensure that the decision process is transparent, based on best knowledge and reflecting the common understanding of stakeholders. Using a risk matrix is both a qualitative and quantitative approach to prioritize risk and start interventions to mitigate the risk and to facilitate constructive discussions within a decision process. Nonetheless, given the paradigm, it may be that professionals, policymakers or even patients may decide differently on the same questions raised.Ī risk matrix can be helpful and insightful to agree upon new or changed interventions as they present complex risk data in a concise visual and mathematical way.
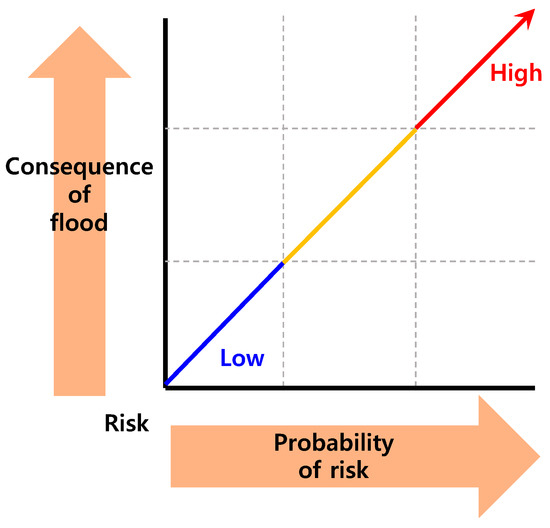
When deciding upon new interventions or strategies, these novel actions should at least prevent or lower the risk of an adverse event to occur. In any case, an intervention is expected to change risk. A newly introduced intervention may decrease the probability of an event to happen and/or can have an effect on its impact. Some interventions have a diagnostic character, whereas others have a preventive or therapeutic effect. In healthcare, prior to introducing a new intervention or diagnostic threshold, professionals and policy makers have to consider what level of risk they would accept and what the expected effect of a newly introduced intervention is. Nonetheless, risk is an objective existence which can never be eliminated, is abrupt and often harmful with people suffering loss, may be uncertain in whether and when the event will happen, and is constantly developing with science and technology. Therefore, decisions are affected by estimating chances and taking the characteristics of these taken chances into account. The impact of that event can be either beneficial or detrimental, ranging from minor to major. However, risk is generally described as the combination of the linked likelihood of occurrence times the impact of a certain event. Although objectively presented data structured group discussions, decisions in guideline development are affected by several other factors than risk reduction alone.ĭuring clinical guideline development, healthcare professionals discuss risk and usually weigh the probability of an event occurring. Professionals are willing to change policies at much lower level of anticipated effectiveness than defined upfront. Professionals weighed other aspects besides risk reduction, as financial aspects and practical consequences for daily practice in this guideline-making process. Nonetheless, when making guidelines, interventions were introduced without reaching the predefined threshold of desired risk reduction. Upfront, professionals opinioned that non-invasive interventions should decrease the general population risk, whereas invasive interventions should decrease the risk in high-risk groups. Second, qualitative assessment of possible additional factors affecting final decisions, that followed from group discussion and guideline development were evaluated. First, professionals’ opinion on required performance characteristics on risk were evaluated by a qualitative online survey. A risk matrix showed the probability and impact of an intervention, together with the corresponding risk category.

To improve care outcomes, we developed new guidelines in which care professionals had to decide upon novel interventions and diagnostic thresholds. We evaluated the effect of interventions and diagnostic thresholds on modeled risk, by using the risk matrix approach (RMA) in a clinical guideline development process, and investigated which additional factors affected choices. This combination of probability and impact can be visualized in a risk matrix. However, in daily practice, risk is perceived as the combination of probability and the impact of desired and adverse events. Clinical guidelines are developed to lower risks, mostly viewed upon as probability.


 0 kommentar(er)
0 kommentar(er)
